[vc_row type=”full_width_content” full_screen_row_position=”middle” equal_height=”yes” content_placement=”middle” bg_color=”#ffffff” scene_position=”center” text_color=”light” text_align=”left” overlay_strength=”0.3″ shape_divider_position=”bottom” bg_image_animation=”none”][vc_column column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_link_target=”_self” column_shadow=”none” column_border_radius=”none” width=”1/1″ tablet_width_inherit=”default” tablet_text_alignment=”center” phone_text_alignment=”center” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”]
Peptic Ulcer Disease (PUD)
[/vc_column_text][/vc_column_inner][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/3″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none” alignment=”right”][mpc_button preset=”mpc_preset_26″ url=”url:%23modal_id_reviewers|||” font_preset=”default” font_color=”#ffffff” font_size=”13″ font_line_height=”1.3″ font_transform=”uppercase” font_align=”right” title=”Reviewers” icon_size=”14″ background_color=”#555555″ border_css=”border-width:0px;border-color:#444444;border-style:solid;border-radius:3px;” padding_divider=”true” padding_css=”padding-top:8px;padding-right:8px;padding-bottom:8px;padding-left:8px;” margin_divider=”true” margin_css=”margin-top:10px;margin-right:2px;” hover_background_color=”#333333″ hover_border_css=”border-color:#444444;border-style:solid;”][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”none” text_align=”left” css=”.vc_custom_1565287910523{margin-top: -20px !important;}”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][mpc_button preset=”mpc_preset_26″ url=”url:%23modal_id_5ced944b48d3f|||” font_preset=”default” font_color=”#ffffff” font_size=”13″ font_line_height=”1.3″ font_transform=”uppercase” title=”Quick Review” icon_size=”14″ background_color=”#555555″ border_css=”border-width:0px;border-color:#444444;border-style:solid;border-radius:3px;” padding_divider=”true” padding_css=”padding-top:8px;padding-right:8px;padding-bottom:8px;padding-left:8px;” margin_divider=”true” margin_css=”margin-top:10px;margin-right:2px;” hover_background_color=”#333333″ hover_border_css=”border-color:#444444;border-style:solid;”][mpc_button preset=”mpc_preset_26″ url=”url:%23modal_id_brochure|||” font_preset=”default” font_color=”#ffffff” font_size=”13″ font_line_height=”1.3″ font_transform=”uppercase” title=”Patient Brochure” icon_size=”14″ background_color=”#555555″ border_css=”border-width:0px;border-color:#444444;border-style:solid;border-radius:3px;” padding_divider=”true” padding_css=”padding-top:8px;padding-right:8px;padding-bottom:8px;padding-left:8px;” margin_divider=”true” margin_css=”margin-top:10px;margin-right:2px;” hover_background_color=”#333333″ hover_border_css=”border-color:#444444;border-style:solid;”][/vc_column_inner][/vc_row_inner][mpc_modal preset=”mpc_preset_5″ frequency=”onclick” onclick_id=”modal_id_5ced944b48d3f” max_width=”75″ max_height=”75″ position=”bottom-center” close_overlay=”true” mpc_icon__transition=”fade” mpc_icon__icon=”eti eti_close” mpc_icon__icon_color=”#555555″ mpc_icon__icon_size=”24″ mpc_icon__background_color=”#f3f3f3″ mpc_icon__border_css=”border-width:1px;border-color:#f3f3f3;border-style:solid;border-radius:99px;” mpc_icon__padding_css=”padding:10px;” mpc_icon__margin_divider=”true” mpc_icon__margin_css=”margin-top:-40px;margin-right:-40px;” mpc_icon__hover_icon_color=”#333333″ mpc_icon__hover_background_color=”#e5e5e5″ mpc_icon__hover_border_css=”border-width:5px;border-color:#e5e5e5;border-style:solid;border-radius:99px;” overlay_background_color=”rgba(48,48,48,0.48)” background_color=”#f7f7f7″ border_css=”border-width:15px;border-color:#e5e5e5;border-style:solid;” padding_css=”padding:40px;” animation_in_type=”transition.slideDownBigIn” animation_in_offset=”100″ animation_in_duration=”1200″ animation_in_delay=”1000″][vc_column_text]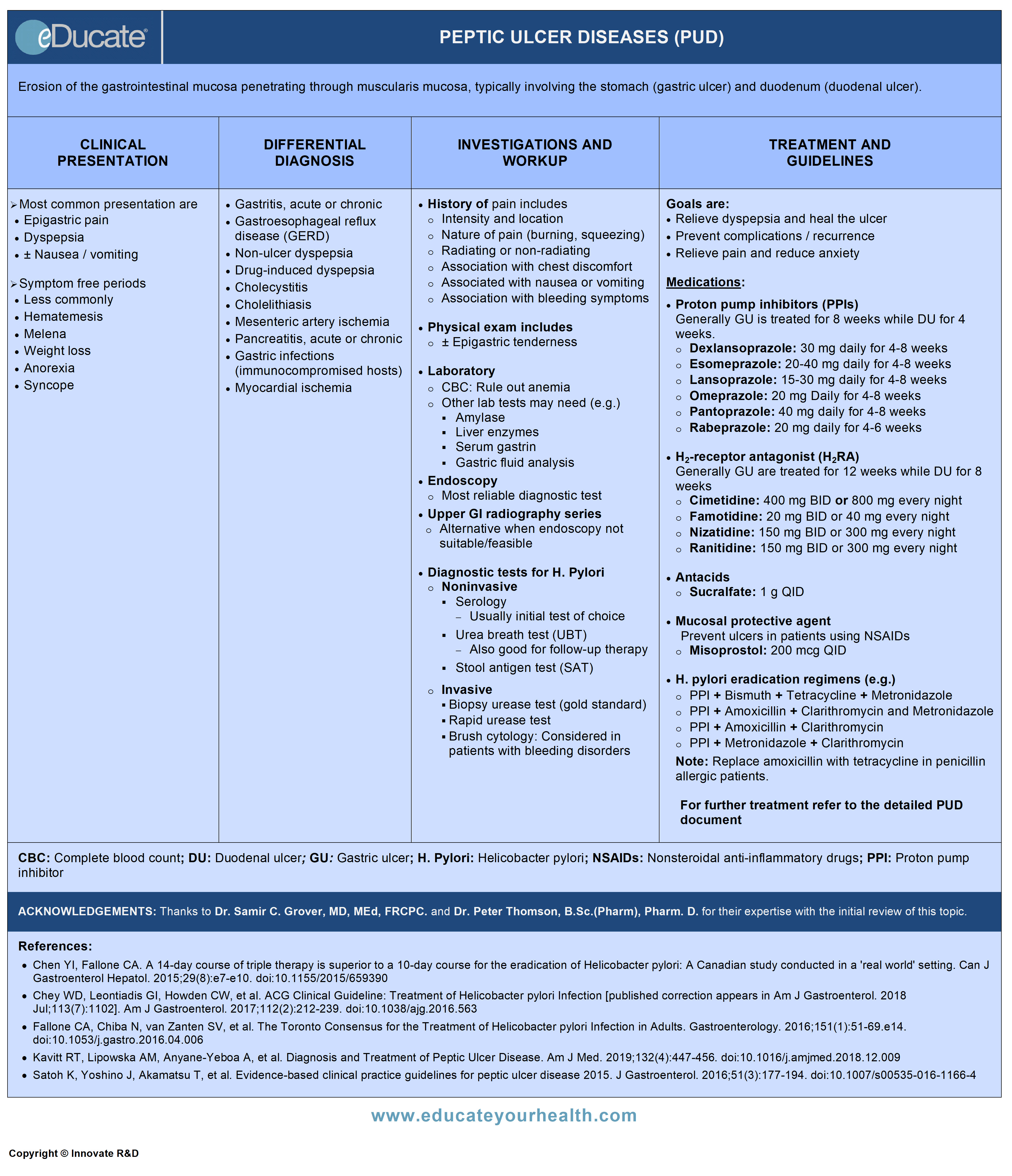 [/vc_column_text][/mpc_modal][mpc_modal preset=”mpc_preset_5″ frequency=”onclick” onclick_id=”modal_id_reviewers” max_width=”40″ max_height=”40″ mpc_icon__transition=”fade” mpc_icon__icon=”eti eti_close” mpc_icon__icon_color=”#555555″ mpc_icon__icon_size=”24″ mpc_icon__background_color=”#f3f3f3″ mpc_icon__border_css=”border-width:1px;border-color:#f3f3f3;border-style:solid;border-radius:99px;” mpc_icon__padding_css=”padding:10px;” mpc_icon__margin_divider=”true” mpc_icon__margin_css=”margin-top:-40px;margin-right:-40px;” mpc_icon__hover_icon_color=”#333333″ mpc_icon__hover_background_color=”#e5e5e5″ mpc_icon__hover_border_css=”border-width:5px;border-color:#e5e5e5;border-style:solid;border-radius:99px;” overlay_background_color=”rgba(48,48,48,0.48)” background_color=”#f7f7f7″ border_css=”border-width:15px;border-color:#e5e5e5;border-style:solid;” padding_css=”padding:40px;” animation_in_type=”transition.slideDownBigIn” animation_in_offset=”100″ animation_in_duration=”1200″ animation_in_delay=”1000″][vc_column_text]ACKNOWLEDGEMENTS:
[/vc_column_text][/mpc_modal][mpc_modal preset=”mpc_preset_5″ frequency=”onclick” onclick_id=”modal_id_reviewers” max_width=”40″ max_height=”40″ mpc_icon__transition=”fade” mpc_icon__icon=”eti eti_close” mpc_icon__icon_color=”#555555″ mpc_icon__icon_size=”24″ mpc_icon__background_color=”#f3f3f3″ mpc_icon__border_css=”border-width:1px;border-color:#f3f3f3;border-style:solid;border-radius:99px;” mpc_icon__padding_css=”padding:10px;” mpc_icon__margin_divider=”true” mpc_icon__margin_css=”margin-top:-40px;margin-right:-40px;” mpc_icon__hover_icon_color=”#333333″ mpc_icon__hover_background_color=”#e5e5e5″ mpc_icon__hover_border_css=”border-width:5px;border-color:#e5e5e5;border-style:solid;border-radius:99px;” overlay_background_color=”rgba(48,48,48,0.48)” background_color=”#f7f7f7″ border_css=”border-width:15px;border-color:#e5e5e5;border-style:solid;” padding_css=”padding:40px;” animation_in_type=”transition.slideDownBigIn” animation_in_offset=”100″ animation_in_duration=”1200″ animation_in_delay=”1000″][vc_column_text]ACKNOWLEDGEMENTS:
Thanks to Dr. Samir C. Grover, MD, MEd, FRCPC, Consultant, Division of Gastroenterology, St. Michael’s Hospital, Assistant Professor, Department of Medicine, University of Toronto, ON Canada and Dr. Peter Thomson, B.Sc.(Pharm), Pharm. D., Clinical Pharmacist, Health Sciences Centre, Winnipeg, MB Canada for their expertise with the initial review of this topic.[/vc_column_text][/mpc_modal][mpc_modal preset=”mpc_preset_5″ frequency=”onclick” onclick_id=”modal_id_brochure” max_width=”75″ max_height=”75″ position=”bottom-center” close_overlay=”true” mpc_icon__transition=”fade” mpc_icon__icon=”eti eti_close” mpc_icon__icon_color=”#555555″ mpc_icon__icon_size=”24″ mpc_icon__background_color=”#f3f3f3″ mpc_icon__border_css=”border-width:1px;border-color:#f3f3f3;border-style:solid;border-radius:99px;” mpc_icon__padding_css=”padding:10px;” mpc_icon__margin_divider=”true” mpc_icon__margin_css=”margin-top:-40px;margin-right:-40px;” mpc_icon__hover_icon_color=”#333333″ mpc_icon__hover_background_color=”#e5e5e5″ mpc_icon__hover_border_css=”border-width:5px;border-color:#e5e5e5;border-style:solid;border-radius:99px;” overlay_background_color=”rgba(48,48,48,0.48)” background_color=”#f7f7f7″ border_css=”border-width:15px;border-color:#e5e5e5;border-style:solid;” padding_css=”padding:40px;” animation_in_type=”transition.slideDownBigIn” animation_in_offset=”100″ animation_in_duration=”1200″ animation_in_delay=”1000″][vc_column_text]
[/vc_column_text][/mpc_modal][mpc_modal preset=”mpc_preset_5″ frequency=”onclick” onclick_id=”modal_id_video” max_width=”65″ max_height=”85″ mpc_icon__transition=”fade” mpc_icon__icon=”eti eti_close” mpc_icon__icon_color=”#555555″ mpc_icon__icon_size=”24″ mpc_icon__background_color=”#f3f3f3″ mpc_icon__border_css=”border-width:1px;border-color:#f3f3f3;border-style:solid;border-radius:99px;” mpc_icon__padding_css=”padding:10px;” mpc_icon__margin_divider=”true” mpc_icon__margin_css=”margin-top:-40px;margin-right:-40px;” mpc_icon__hover_icon_color=”#333333″ mpc_icon__hover_background_color=”#e5e5e5″ mpc_icon__hover_border_css=”border-width:5px;border-color:#e5e5e5;border-style:solid;border-radius:99px;” overlay_background_color=”rgba(48,48,48,0.48)” background_color=”#f7f7f7″ border_css=”border-width:15px;border-color:#e5e5e5;border-style:solid;” padding_css=”padding:40px;” animation_in_type=”transition.slideDownBigIn” animation_in_offset=”100″ animation_in_duration=”1200″ animation_in_delay=”1000″][vc_column_text]
[/vc_column_text][/mpc_modal][divider line_type=”Full Width Line” line_thickness=”1″ divider_color=”default” custom_height=”30″][/vc_column][/vc_row][vc_row type=”in_container” full_screen_row_position=”middle” scene_position=”center” text_color=”dark” text_align=”left” top_padding=”10″ class=”zindexbottom elementup” overlay_strength=”0.3″ shape_divider_position=”bottom” bg_image_animation=”none” shape_type=””][vc_column column_padding=”no-extra-padding” column_padding_position=”all” background_color=”#fcfcfc” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_link_target=”_self” column_shadow=”none” column_border_radius=”none” width=”1/1″ tablet_width_inherit=”default” tablet_text_alignment=”default” phone_text_alignment=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_row_inner column_margin=”default” text_align=”left” el_id=”definition-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Definition
[/vc_column_text][vc_column_text]Erosion of the gastrointestinal mucosa extending through the muscularis layer, involving the stomach (gastric ulcer), and duodenum (duodenal ulcer).[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”etiology-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Etiology
[/vc_column_text][vc_column_text]Common causes:
- Helicobacter pylori (H. pylori) infection
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
Less common causes:
- Other drugs may include steroids, bisphosphonates
- Carcinoid syndrome
- Post-gastric surgery
- Chronic renal failure
- Radiation/chemotherapy
- Zollinger-Ellison syndrome
- Crohn’s disease
- Ischemia, usually related to crack cocaine use
Risk factors:
- Smoking/stress
- Diabetes mellitus
- Cirrhosis
[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”epidemiology-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Epidemiology
[/vc_column_text][vc_column_text]
- Annual incidence of PUD ranges from 0.1-0.3%
- Incidence increases with age
- Incidence in H. pylori-infected individuals is ~1% per year
- 70% of ulcers occur between ages 25 and 64 years
- No predilection by gender
- First-degree relatives of patients with duodenal ulcer (DU) have a threefold increase in the prevalence of DU but not gastric ulcer (GU)
- Lifetime prevalence is 8-14%; 20% higher in H. pylori positive subjects
- Mortality rate is approximately 1 death per 100,000 cases
- Hospitalization rate is 30 patients per 100,000 cases
[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”pathophysiology-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Pathophysiology
[/vc_column_text][vc_column_text]Parietal cells of stomach produce acid and decrease pH, which in turn causes the release of somatostatins leading to inhibition of acid secretion (by negative feedback control).
Within the acidic environment of the stomach, the mucosa is protected by several mechanisms as follows:
- Production of mucus and HCO3 where mucus serves as a barrier to acid diffusion
- Epithelial cells remove excess H+ ions and prevent back diffusion
- Mucosal blood flow removes excess acid
- Growth factors and prostaglandins are shown to have protective effects
Factors that interfere with these mucosal defenses (particularly NSAIDs and Helicobacter pylori infection) predispose to gastritis and peptic ulcer disease.
NSAIDs cause mucosal inflammation and ulcer formation by:
- Inhibiting prostaglandin production by blocking enzyme cyclooxygenase (COX)
- Reduce gastric blood flow causing decreased cell repair and replication
- They are weak acids, diffuse freely across the mucous membrane, liberating H+ ions leading to cellular damage
Helicobacter pylori: Interferes with mucosal physiology mechanisms include
- Increase acid secretion (combination of increase in acid secretions and decrease in duodenal bicarb secretion resulting in low pH)
- Gastric metaplasia is promoted by increased acid secretion
- Alters immune responses leading to persistent colonization
- H. pylori colonization in duodenum induces inflammation and reduces bicarb secretion thus promoting ulcer formation
- Diminishes mucosal defense mechanism
[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”clinical-presentation-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Clinical Presentation
[/vc_column_text][vc_column_text]General symptoms:
- Epigastric pain
- Dyspepsia
- ± Nausea/vomiting
- Symptom free periods (months to years), alternate with the symptomatic periods (weeks to months)
Other less common symptoms/complications:
- Hematemesis
- Melena
- Weight loss
- Anorexia
- Syncope
GU: Recurrent burning or gnawing pain in the epigastrium (not related to food), heartburn, early satiety, and radiation of pain to the xiphisternum.
DU: Consistent pain, which may awake the patient in the night, related to food (subsides in 50% with food intake, but recur after 2-3 hrs).
 [/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”differential-diagnosis-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”differential-diagnosis-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Differential Diagnosis
[/vc_column_text][vc_column_text]
- Gastritis, acute or chronic
- Gastroesophageal reflux disease (GERD)
- Non-ulcer dyspepsia
- Drug-induced dyspepsia
- Cholecystitis
- Cholelithiasis
- Mesenteric artery ischemia
- Pancreatitis, acute or chronic
- Gastric infections (immunocompromised hosts)
- Myocardial ischemia
[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”investigation-and-workup-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Investigation and Workup
[/vc_column_text][vc_column_text]HISTORY:
History of pain includes:
- Intensity/location
- Nature of pain (burning, squeezing)
- Radiating or non-radiating
- Association with meals or nausea/vomiting
- Association with chest discomfort
EXAMINATION:
- Epigastric tenderness may or may not be present
LABORATORY:
- CBC, LFTs
- Serum amylase and lipase
- Cardiac enzymes (rule out myocardial ischemia in acute presentation)
- Helicobacter pylori serology
- Serum gastrin
- Gastric fluid analysis
IMAGING STUDIES
Upper gastrointestinal radiography series:
- Indicated when endoscopy is unsuitable or not feasible
- Relatively low sensitivity and specificity
- Avoid in the patient with upper GI bleeding

Esophagogastroduodenoscopy (endoscopy):
Most reliable diagnostic test for PUD
Indications for endoscopy include:
- Patient >50 years with new-onset dyspepsia
- Symptoms of bleeding, weight loss, dysphagia
- Refractory or persistent abdominal pain
- Suspicion of upper GI abnormality (mass, stricture, ulcers, etc.)
- Diagnosis of an H. pylori infection when non-invasive testing is not possible

Screening for H. pylori
Indications:
- History of dyspepsia
- Active or uncomplicated peptic ulcer disease
- Gastric MALT (mucosa-associated lymphoid tissue) lymphoma
- Recent bleeding in PUD patients
- First degree relatives of gastric cancer patients
- Patients with idiopathic thrombocytopenic purpura (ITP)
- Unexplained iron deficiency anemia
Noninvasive diagnostics:
- Serology: ELISA techniques detect IgG antibodies (sensitivity ~60-90%)
- It will not distinguish a previous infection from the current one (i.e., test would be positive if the patient ever had H.pylori); if the test result is negative, it is unlikely that a person ever had an H. pylori infection
- Urea breath test (UBT): Sensitivity and specificity is about >90%
- Discontinue proton pump inhibitors or H2 receptor antagonists, antibiotics and bismuth 4 weeks before a test based on H. pylori urease production
- Stool antigen test (SAT): Sensitivity 91% and specificity 93%
- The use of SATs should only be considered if the UBT is not available
Invasive diagnostics:
Endoscopy:
- Biopsy (gold standard): 95% sensitive / 100% specific / results in 24 hrs
- Rapid urease test: 95% sensitive / 95% specific / results in 1 hr
- Brush cytology: Considered in patients with bleeding disorders; where biopsies are considered undesirable
- Histology helps in distinguishing inflammation, metaplasia, and MALT
- Polymerase Chain reaction (PCR) used only when ordinary culture cannot be done
Confirmation of eradication should be strongly considered and assessed through noninvasive tests (stool and breath tests).[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”treatment-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Treatment
[/vc_column_text][cq_vc_tabs tabsstyle=”style2″ titlebg=”#16847d” titlehoverbg=”#333333″ rotatetabs=”0″][cq_vc_tab_item tabtitle=”Management & Therapies”]Peptic ulcer disease is treated according to its cause:
- H. pylori associated ulcer
- NSAIDs associated ulcers
- Refractory ulcers
1) H. PYLORI ASSOCIATED ULCERS:
The goal is to relieve dyspepsia, promote healing, and cure the infection.
Recommended 1st Line treatment duration is of 14 days quadruple therapy; treatment options are as follows:
Proton pump inhibitors (PPIs):
- Example: Pantoprazole 40 mg PO BID or omeprazole 20 mg PO BID or rabeprazole 20 mg PO BID or lansoprazole 30 mg PO BID or esomeprazole 40 mg once daily or dexlansoprazole 30 mg once daily
Penicillin allergic:
- Replace Amoxicillin with Tetracycline (500 mg) four times a day
1st Line Regimens includes (for 14 days):
Option 1 (PBMT) quadruple therapy:
- PPI standard dose BID plus
- Bismuth subsalicylate 524 mg QID plus
- Metronidazole 500 mg QID plus
- Tetracycline 500 mg QID
Option 2 (PAMC) quadruple therapy:
- PPI standard dose BID plus
- Amoxicillin 1000 mg BID plus
- Metronidazole 500 mg BIDplus
- Clarithromycin 500 mg BID
Restricted option (triple therapy): Restricted to areas with known low clarithromycin resistance (<15%) or proven high local eradication rates (>85%)
- PAC: PPI standard dose BID + Amoxicillin 1000 mg BID + Clarithromycin 500 mg BID
- PMC: PPI standard dose BID + Metronidazole 500 mg BID + Clarithromycin 500 mg BID
2nd Line Regimens: (For 14 days):
When PBMT or PAMC as an initial therapy fails:
- PAL: PPI standard dose BID + Amoxicillin 1000 mg BID + Levofloxacin 500 mg QD
When “Restricted option” (triple therapy) as an initial therapy fails:
- If initial therapy was PAC then go for either PBMT or PAL
- If initial therapy was PMC then initiate PAL
3rdLine Regimens: (For 14 days):
- PBMT quadruple therapy is recommended
- Optimized PBMT (higher dose of PPI and metronidazole) quadruple therapy can be used specially if someone prefers to avoid rifabutin or was already had prior PBMT therapy
- In Restricted option, if one was on PBMT as a 2nd line therapy then use PAL
4thLine Regimens: (For 10 days):
- PAR: PPI standard dose BID + Amoxicillin 1000 mg BID + Rifabutin 150 mg BID
- Note:
- ➣ Should only be considered who have failed to respond to above 3 regimens
- ➣ Rifabutin has rarely been associated with potentially serious myelotoxicity
Complicated ulcers or ulcers >1 cm: Antisecretory agent should be given for an additional 2-4 wks in duodenal ulcers and 4-6weeks in gastric ulcers.
Note: Patients should always be retested for H. pylori eradication after >4 weeks of completion of therapy.
2) NSAID-ASSOCIATED ULCERS:
Active ulcers: Discontinue offending agents if possible.
Treatment options:
PPIs:
- Example: Pantoprazole 40 mg PO BID or omeprazole 20 mg PO BID or rabeprazole 20 mg PO BID or lansoprazole 30 mg PO BID or esomeprazole 40 mg once daily or dexlansoprazole 30 mg PO once daily
- Duodenal ulcers (uncomplicated) treated for 4 weeks
- Gastric ulcers (uncomplicated) treated for 8 weeks
- For complicated ulcers, PPIs are preferred drugs
H2 receptor antagonists:
Uncomplicated duodenal ulcers:
- Cimetidine 800 mg or ranitidine or nizatidine 300 mg or famotidine 40 mg PO daily at bedtime for 6 weeks
Uncomplicated gastric ulcers:
- Cimetidine 400 mg or ranitidine or nizatidine 150 mg or famotidine 20 mg PO twice daily for 8 weeks
3) PREVENTION AND MAINTENANCE:
A) High-risk patients related to NSAID induced ulcer requiring prophylactic therapy include:
- History of ulcers
- Complicated ulcers
- Current use of steroids or anticoagulants/antiplatelet agents
- Age >60 years
- Serious comorbid illness
Treatment Options:
- PPIs
- Change patient to selective COX 2 inhibitors (contraindicated in patients with risk of CVD)
- Misoprostol 200 mcg PO QID
B) Long term maintenance therapy is indicated in patients with recurrent ulcers who are H. pylori negative or have failed attempts of eradication.
Treatment Options:
- PPIs
- H2 receptor antagonist
C) Non-pharmacological therapy includes:
- Quit smoking
- Avoid excess alcohol
- Dietary modification
- Adequate rest
4) COMPLICATIONS OF PEPTIC ULCER:
Perforation (medical emergency)
- Severe sudden abdominal pain
- Rigidity
- Abdominal distension
Treatment options:
- Simple closure
- Graham patch with or without a laparoscopic vagotomy (for duodenal ulcers)
- Truncal vagotomy with pyloroplasty (incorporating the perforation)
- Preferred approach for gastric ulcers in the elderly is partial gastrectomy
Bleeding
- Hemodynamic instability
- Hematemesis/hematochezia/melena
– Initial management
- Resuscitation
- Medical therapy with intravenous proton pump inhibitors
- Rapidly correct coagulopathy with blood products
- Endoscopic intervention
- Injection therapy (options):
- Epinephrine injection
- Saline injection (to tamponade bleeding vessel)
- Fibrin sealant or other injection sclerotherapy
- Injection therapy (options):
- Note: While various agents have been used to help control bleeding a key feature of injection therapy, regardless of agent, is essential to tamponade the bleeding vessel. The use of sclerosants may be complicated by perforations and are usually discouraged.
- Thermal coagulation: May be achieved through direct contact devices (e.g. heater probes, electrocoagulation) and noncontact devices [argon plasma coagulation (APC)], which appear to have similar efficacy
- Endoclips/Hemoclips: May have the distinct advantage of lowering the rate of recurrent bleeding as compared to other therapies, but are difficult to apply and so cannot always be utilized
- Combination therapy: Diluted epinephrine injection followed with thermocoagulation may be a useful approach particularly in high-risk patients
– Indications for surgery
- Hemodynamic instability despite vigorous resuscitation (>3 unit transfusion)
- Shock associated with recurrent hemorrhage
- Failure to arrest hemorrhage on endoscopy
- Recurrent bleeding despite endoscopic attempts at achieving hemostasis
Surgical procedures
- Duodenal ulcers: First ligation of gastroduodenal artery at the superior and inferior aspect of the ulcer is done then pyloroplasty possibly combined with truncal vagotomy
- Gastric ulcers: Resection with Billroth I or II reconstruction
Penetration
- Penetration through the bowel wall without perforation and leakage of luminal contents into the peritoneal cavity
- 20% of ulcers penetrate
- Presents with gradual or sudden change in symptoms
- Gastrocolic fistulae are seen with greater curvature gastric ulcers
Treatment
- Managed with intensive ulcer treatment regimens
- Surgical options can also be considered
Obstruction
- Early satiety and bloating
- Indigestion/epigastric pain
- Anorexia/weight loss
- Nausea and vomiting of recognizable food
- Dehydration/metabolic alkalosis
Treatment
Gastric outlet obstruction is usually not an emergency.
Stabilize patient then consider:
- Nasogastric tube decompression
- Correction of fluid and electrolyte
- Preoperative nutritional supplementation
- Full dose intravenous antisecretory therapy
- Endoscopic balloon dilatation
- Surgical options are:
- Truncal vagotomy and gastrojejunostomy
- Antrectomy (rarely performed)
- Distal gastrectomy, combined with vagotomy
[/cq_vc_tab_item][cq_vc_tab_item tabtitle=”Medication Dose”]Medications:
- Cimetidine
- Famotidine
- Nizatidine
- Ranitidine
MECHANISM:
Inhibits the histamine at H2 receptors of the gastric parietal cells, resulting in decreased secretion of gastric acid.
DOSE:
Cimetidine
- Oral: 400 mg BID or 800 mg once daily
- strong>IV / IM: 300 mg every 6 hrs; Dilute for IV route
Dose in renal insufficiency:
- Decrease dose by 50% if ClCr 10-50 mL/min
- Decrease dose by 75% if ClCr <10 mL/min
Famotidine
- Oral: 20 mg BID or 40 mg daily
- IV: 20 mg every 12 hrs
Dose in renal insufficiency:
- Decrease dose by 50% if ClCr <50 mL/min
Nizatidine
- Oral: 150 mg BID or 300 mg daily
Dose in renal impairment:
Active treatment:
- Clcr 20-50 mL/minute: 150 mg/day
- Clcr <20 mL/minute: 150 mg every other day
Maintenance treatment:
- Clcr 20-50 mL/minute: 150 mg every other day
- Clcr <20 mL/minute: 150 mg every 3 days
Ranitidine
- Oral: 150 mg BID or 300 mg once daily
- IV / IM: 50 mg every 6-8 hrs; dilute for IV route
Dose in renal insufficiency:
- 150 mg PO daily; if ClCr <50 mL/min
- Dexlansoprazole
- Esomeprazole
- Lansoprazole
- Omeprazole
- Pantoprazole
- Rabeprazole
MECHANISM:
Suppress gastric acid secretion by inhibition of the gastric enzyme H+/K+-ATPase in the gastric parietal cell.
DOSE:
Dexlansoprazole
- Healing of erosive esophagitis: 60 mg PO once daily for up to 8 weeks
- Maintenance of healed erosive esophagitis: 30 mg PO once daily
- Symptomatic non-erosive gastroesophageal reflux disease: 30 mg PO once daily for 4 weeks
Esomeprazole
- Oral: 20-40 mg daily for 4-8 weeks
- IV: 20-40 mg daily
Lansoprazole
- Duodenal ulcer: 15 mg PO daily for ~4 weeks
- Gastric ulcer: 30 mg PO daily for ~8 weeks
- IV: 30 mg IV daily over 30 min
Omeprazole
- 20 mg PO once daily for 4-8 weeks.; in refractory patients 40 mg PO daily
Pantoprazole
- 40 mg PO daily for 4-8 weeks
Rabeprazole
- 20 mg PO daily for 4-6 weeks
Gastroduodenal Cytoprotective Agent-Antacids
- Sucralfate
MECHANISM:
Produces an adherent and cytoprotective barrier at the ulcer site by binding with positively charged proteins in exudates, forming a protective coat for ulcer site against peptic acid, pepsin, and bile.
DOSE:
Sucralfate
Peptic ulcer
- 1 g PO QID, an hour before meals and at bedtime, on an empty stomach for 4-8 weeks
Duodenal ulcer
- 2 g PO BID on waking up and at bedtime on an empty stomach for 4-8 weeks
Duodenal ulcer maintenance/prophylaxis
- 1 g PO BID on an empty stomach
- Misoprostol
MECHANISM:
It is a synthetic analog of prostaglandin E1.
- It replaces the protective prostaglandins that have been depleted due to prostaglandin-inhibiting therapies (e.g. NSAIDs) and also inhibits the acid production
- It also induces uterine contractions and exhibits a significant cervical priming effect
DOSE:
Misoprostol
Duodenal ulcers/Prevention of NSAID-induced ulcers
- 200 mcg PO QID with food and fourth dose taken at bedtime; if not tolerated, may decrease dose to 100 mcg QID or 200 mcg BID
Note: Administer for the duration of NSAID therapy
[/cq_vc_tab_item][/cq_vc_tabs][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”clinical-trials-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Clinical Trials
[/vc_column_text][vc_column_text]
- Clopidogrel and the Optimization of Gastrointestinal Events (COGENT-1)
- Effect of intravenous omeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers
- Eradication of Helicobacter pylori and risk of peptic ulcers in patients starting long-term treatment with non-steroidal anti-inflammatory drugs: a randomised trial.
[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”pipe-line-agents-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Pipeline Agents
[/vc_column_text][vc_column_text]Pending new data[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”physician-resources-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
Physician Resources
[/vc_column_text][vc_column_text]1. Tips for patient care
General management:
- When diagnosing peptic ulcer disease, important considerations are on detecting H. pylori infection, NSAID and/or aspirin use, and an acid hypersecretory state
- Understanding the pathophysiology and optimal treatment of non-NSAID, non-H. pylori associated peptic ulcers is an important focus for future research
- Educate patient about
- Signs, symptoms, and therapy
- Advise small and frequent meals
- Effects of alcohol consumption, smoking, and stress
- Testing for and eradicating H. pylori infection is recommended before starting NSAIDs and in those taking NSAIDs who have a history of ulcers or ulcer complications
- Strategies to quit smoking be discussed with smokers
- Consider repeating UBT or endoscopy to confirm the eradication of H. Pylori in patients with complicated ulcer
- Educate about the signs and symptoms of bleeding and when to notify the health care provider
- Risk of rebleeding, NSAID ulcer recurrence and ulcer relapse rate are decreased after H. pylori eradication
Medications:
- For patients at risk of developing an ulcer or ulcer complications, the choice of anti-inflammatory drugs, nonselective or COX2-selective NSAIDs should be carefully made
- The first-line choice for H. pylori eradication is combination treatment with antisecretory drugs and antibiotics for 14 days
- Evaluate cost, affordability and insurance coverage for patients
- If possible, use alternate options to salicylates and NSAIDs
- For patients on NSAID, discuss the risk of NSAID-induced gastric complications
- Consider concurrent risk factors and disease states with the prescribed therapy
- Adherence to treatment should be assessed at each visit
Social and Stress factors:
- Explain all tests and procedures to minimize anxiety
Activities (Physical, Mental, others):
- Emphasize patients, importance of staying active and having a regular healthy diet
- Advise to keep positive attitude
2. Scales and Tables
- Clinical comparison of gastric ulcer and duodenal ulcer
- Radiographic differentiation of benign versus malignant lesions
- Differentiation of benign gastric ulcers from cancer at endoscopy
[/vc_column_text][/vc_column_inner][/vc_row_inner][vc_row_inner column_margin=”default” text_align=”left” el_id=”references-title”][vc_column_inner column_padding=”no-extra-padding” column_padding_position=”all” background_color_opacity=”1″ background_hover_color_opacity=”1″ column_shadow=”none” column_border_radius=”none” column_link_target=”_self” width=”1/1″ tablet_width_inherit=”default” column_border_width=”none” column_border_style=”solid” bg_image_animation=”none”][vc_column_text]
References
[/vc_column_text][vc_column_text]Core Resources:
- Chen YI, Fallone CA. A 14-day course of triple therapy is superior to a 10-day course for the eradication of Helicobacter pylori: A Canadian study conducted in a ‘real world’ setting. Can J Gastroenterol Hepatol. 2015;29(8):e7-e10. doi:10.1155/2015/659390
- Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection [published correction appears in Am J Gastroenterol. 2018 Jul;113(7):1102]. Am J Gastroenterol. 2017;112(2):212-239. doi:10.1038/ajg.2016.563
- Compendium of Pharmaceuticals and Specialties (CPS). Canadian Pharmacist Association. Toronto: Webcom Inc. 2012
- Day RA, Paul P, Williams B, et al (eds). Brunner & Suddarth’s Textbook of Canadian Medical-Surgical Nursing. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2010
- Fallone CA, Chiba N, van Zanten SV, et al. The Toronto Consensus for the Treatment of Helicobacter pylori Infection in Adults. Gastroenterology. 2016;151(1):51-69.e14. doi:10.1053/j.gastro.2016.04.006
- Foster C, Mistry NF, Peddi PF, Sharma S, eds. The Washington Manual of Medical Therapeutics. 33rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010
- Gray J, ed. Therapeutic Choices. Canadian Pharmacists Association. 6th ed. Toronto: Webcom Inc. 2011
- Holbrook AM (Chair) for Ontario GI Therapy Review Panel. Ontario Guidelines for Peptic Ulcer Disease and Gastroesophageal Reflux. Toronto. First Edition. Queen’s Printer of Ontario, 2000
- Hurst’s the Heart Manual of Cardiology, 12th Edition
- Katzung BG, Masters SB, Trevor AJ, eds. Basic and Clinical Pharmacology. 11th ed. New York: McGraw-Hill; 2009
- Longo D, Fauci A, Kasper D, et al (eds). Harrison’s Principles of Internal Medicine. 18thed. New York: McGraw-Hill; 2011
- McPhee SJ, Papadakis MA, eds. Current Medical Diagnosis & Treatment. 49th ed. New York: McGraw-Hill; 2010
- Pagana KD, Pagana TJ eds. Mosby’s Diagnostic and Laboratory Test Reference. 9th ed. St. Louis: Elsevier-Mosby; 2009
- Skidmore-Roth L. ed. Mosby’s drug guide for nurses. 9th ed. St. Louis: Elsevier-Mosby; 2011
- Skidmore-Roth L, ed. Mosby’s nursing drug reference. 24th ed. St. Louis: Elsevier-Mosby; 2011
- Yuan Y, Ford AC, Khan KJ, et al. Optimum duration of regimens for Helicobacter pylori eradication. Cochrane Database Syst Rev. 2013;(12):CD008337. Published 2013 Dec 11. doi:10.1002/14651858.CD008337.pub2
Online Pharmacological Resources:
- e-Therapeutics
- Lexicomp
- RxList
- Epocrates
Journals/Clinical Trials:
- Bhatt DL, Cryer BL, Constant CF, et al. Clopidogrel with or without Omeprazole in Coronary Artery Disease N Engl J Med 2010; 363:1909-1917
- Chan FKL, To KF, Wu JCY et al. outline goes here Eradication of Helicobacter pylori and risk of peptic ulcers in patients starting long-term treatment with non-steroidal anti-inflammatory drugs: a randomized trial. The Lancet, 2002 ;(359), pgs.9-13
- Chau CH et al. Randomized controlled trial comparing epinephrine injection plus heat probe coagulation versus epinephrine injection plus argon plasma coagulation for bleeding peptic ulcers. 2003; Gastrointest Endosc 57: 455-461
- Kavitt RT, Lipowska AM, Anyane-Yeboa A, Gralnek IM. Diagnosis and Treatment of Peptic Ulcer Disease. Am J Med. 2019;132(4):447-456. doi:10.1016/j.amjmed.2018.12.009
- Khuroo MS, Yattoo GN, Javid G et al. A comparison of omeprazole and placebo for bleeding peptic ulcer. N Engl J Med. 1997;336(15):1054-8
- Kubba AK, Palmer KR. Role of endoscopic injection therapy in the treatment of bleeding peptic ulcer. Br J Surg 1996; 83:461
- Lai KC, Hui WM, Wong BC, et al. A retrospective and prospective study on the safety of discharging selected patients with duodenal ulcer bleeding on the same day as endoscopy. Gastrointest Endosc. 1997; 45:26
- Lau J.Y.W., Sung J.J.Y., Lee K.K.C., et al. Effect of Intravenous Omeprazole on Recurrent Bleeding after Endoscopic Treatment of Bleeding Peptic Ulcers N Engl J Med 2000; 343:310-316
- Li BZ, Threapleton DE, Wang JY, et al. Comparative effectiveness and tolerance of treatments for Helicobacter pylori: systematic review and network meta-analysis. BMJ. 2015;351:h4052. Published 2015 Aug 19. doi:10.1136/bmj.h4052
- Marshall BJ, Warren JR et al. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1(8390):1311-5
- Park CH, Joo YE, Kim HS, et al. A prospective, randomized trial comparing mechanical methods of hemostasis plus epinephrine injection to epinephrine injection alone for bleeding peptic ulcer. Gastrointest Endosc 2004; 60:173
- Satoh K, Yoshino J, Akamatsu T, et al. Evidence-based clinical practice guidelines for peptic ulcer disease 2015. J Gastroenterol. 2016;51(3):177-194. doi:10.1007/s00535-016-1166-4
- Vaira D, Zullo A, Vakil N et al. Sequential therapy versus standard triple drug therapy for H.pylori eradication: a randomized trial. Ann Intern Med. 2007;146(8):556-63
[/vc_column_text][/vc_column_inner][/vc_row_inner][/vc_column][/vc_row]
